Gene editing has been around for years and is consistently paving the path for curing countless diseases that affect millions of people worldwide. Type 1 Diabetes Mellitus is no exception to said diseases. With over half a million newly diagnosed cases in 2024, the demand for a cure is higher than ever1,2. The transplantation of allogeneic islet cells was previously performed in selected patients with insulin-dependent diabetes. While the technique showed reassuring results in terms of glycemic control, the main drawback was the years-long immunosuppressive protocol that the participants were placed on2,5. This inspired the use of clustered regularly interspaced short palindromic repeats (CRISPR) and CRISPR associated proteins to genetically edit cells, helping them elude the host's immune system and eliminating the need for immunosuppression and its adverse effects6. After some promising results from similar allogeneic transplantations in diabetic humanized mice and the quadriceps of a diabetic monkey, Dr. Carlsson and the team at Uppsala University Hospital decided to apply the approach to humans in a first-in-human, proof-of-concept study4,6,7.
CRISPR, CRISPR-associated protein 12b (Cas12b) and lentiviral transduction were used to modify pancreatic islet cells collected from a human donor and form hypoimmune platform (HIP) islet cells. This was done by depleting HLA class I and HLA class II on cells to avoid damage by T-lymphocytes and increasing the expression of the CD47 surface protein to avoid damage by the innate immune system (macrophages and natural killer cells). The resulting product, called UDP421, contained three main versions of islet cells: HIP islet cells, double-knockout cells (cells that had full HLA depletion but normal CD47 expression) and wild-type islet cells (cells that still expressed HLA).
It is important to note that the process of gene editing did not alter the composition of the donor sample so that the majority of cells (66%) were still insulin-producing beta cells. UDP421 was then transplanted into the brachioradialis muscle of a 42-year-old male with type 1 diabetes. This was done by multiple injections administered directly into the muscle through a small forearm incision while the patient was under general anesthesia. The patient was not placed on any immunosuppressive therapy4.
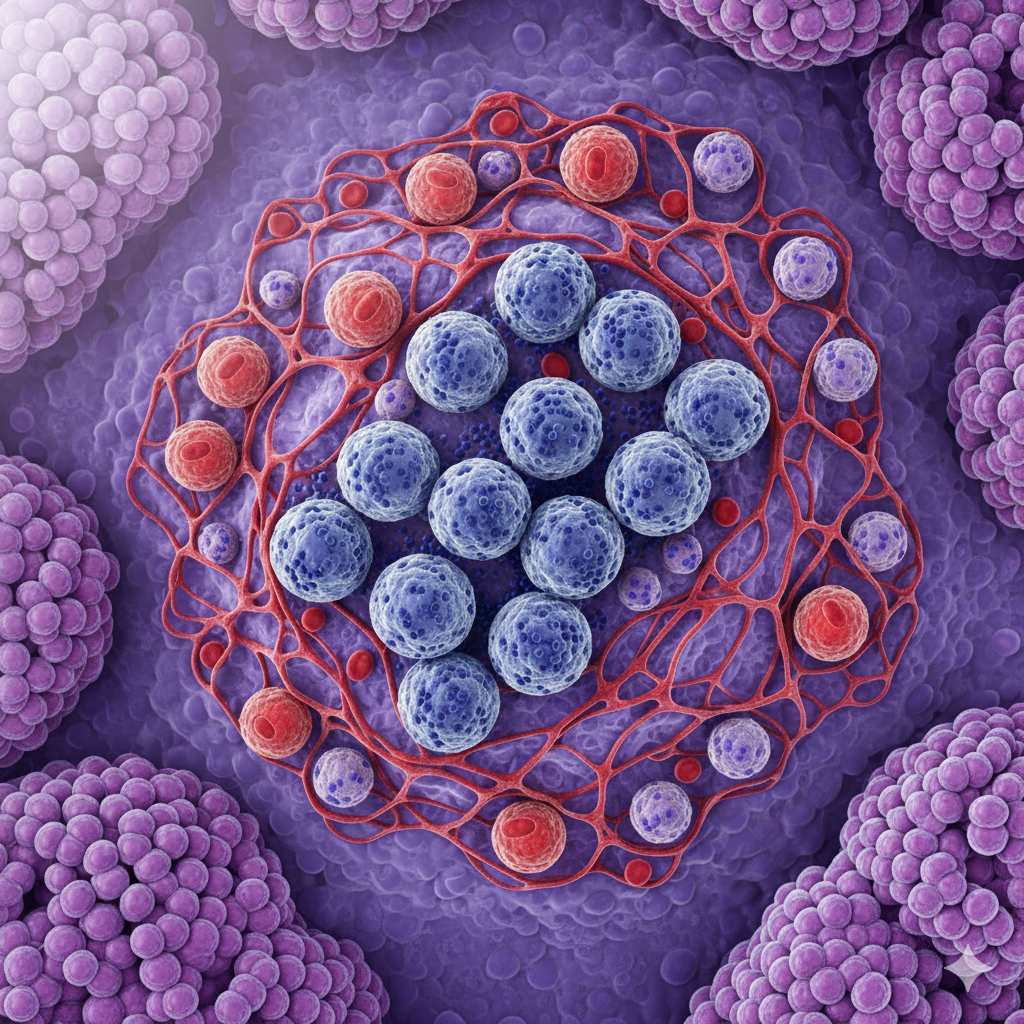
While an immune response was triggered by the double-knockout and the wild-type components, the modified HIP islet cells successfully evaded the immune system and were left unaffected. Moreover, serial measurements of C-peptide levels taken over the span of 12 weeks (a serum biomarker) indicate functional beta cells with stable insulin production. The graft site was additionally monitored by scans that confirmed absence of inflammation and good vascularization. This supports the use of muscle as viable tissue for graft transplantation.
The results from the study were incredibly promising for proof-of-concept, but it is merely the beginning. It should be mentioned that the mass of islet cells used here was only about 7% of what is actually needed to achieve insulin-independence (this was done on purpose due to the regulations specifies for a first-in-human study). The team also believes that more than one HIP graft will be needed to adjust for insulin-dependence. Furthermore, the study used pancreatic cells from a human donor which cannot be a reliable source to supply all type 1 diabetes patients. A possible solution could involve stem cell-derived islet cells, which can be produced and engineered on a larger scale. It is also important to note that the study involved a single patient who was monitored for a few weeks so it could still be early for any significant complications or side effects4.
In conclusion, while some may call it preliminary, the work done by Dr. Carlsson and his team is very reassuring. It strongly suggests that genetically modified pancreatic islet cells can indeed be the secret to achieving insulin-independence in type 1 diabetes patients without the morbidity associated with immunosuppression. Although we still have a long way to go, we are one step closer to curing diabetes.